Abstract
Background : Neutrophil lymphocyte Ratio (NLR)
and Platelet lymphocyte Ratio (PLR) are an indicator
of the status of inflammation. The objective of this
study was to evaluate the relationship between
recipient pre-operative Neutrophil lymphocyte
Ratio (NLR) and Platelet lymphocyte Ratio (PLR)
with delayed graft function in the kidney transplant
patient.
Methods: The preoperative full blood
count, data regarding patient demographics and
postoperative graft function was retrospectively
evaluated from the database of our institution.
All statistical calculations were carried out using
SPSS 20.0 version(SPSS Inc., Chicago, IL,
USA).A p-value<0.05 was considered statistically
significant.
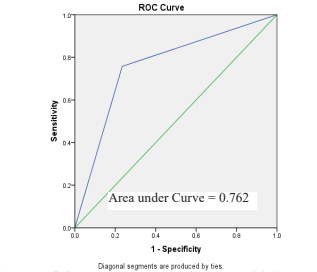
Results: 289 patients were included
in this study. DGF occurred in 33 cases. Elevated
preoperative NLR had a sensitivity of 75.75% and
specificity of 76.56% whereas elevated preoperative
PLR had a sensitivity of 72.72% and specificity of
58.20% for predicting DGF. The area under the ROC
curve was found to be 0.762 and 0.655 for NLR and
PLR, respectively. Multivariate analysis showed
NLR>3.5 and PLR>120 independently responsible
for DGF.
Conclusion: Recipient preoperative
NLR and PLR can predict the occurrence of DGF
following DBD renal transplantation. In addition,
NLR is better than PLR in predicting DGF. DGF
prolongs the total ICU and in-hospital stay.
References
function on graft and patient survival in
kidney transplantation: An approach using
competing events analysis. Transpl. Int.28,
738–750 (2015).
2. Halazun, K. J. et al. Elevated preoperative
recipient neutrophil-lymphocyte ratio is
associated with delayed graft function
following kidney transplantation. Transplant.
Proc.45, 3254–3257 (2013).
3. Fung, A., Zhao, H., Yang, B., Lian, Q. &
Ma, D. Ischaemic and inflammatory injury
in renal graft from brain death donation : an
update review. J. Anesth.30, 307–316 (2016).
4. Helfer, M. S., Vicari, A. R., Spuldaro, F., Gonçalves, L. F. S. & Manfro, R. C.
Incidence, risk factors, and outcomes of
delayed graft function in deceased donor
kidney transplantation in a brazilian center.
Transplant. Proc.46, 1727–1729 (2014).
5. Butala, N., Reese, P., Doshi, M. & Parikh,
C. Is Delayed Graft Function Causally
Associated with Long-Term Outcomes
after Kidney Transplantation? Instrumental
Variable Analysis. Transplantation95, 1008–
1014 (2013).
6. Nashan, B., Abbud-Filho, M. & Citterio, F.
Prediction, prevention, and management of
delayed graft function: where are we now?
Clin. Transplant.30, 1198–1208 (2016).
7. Hayashi, H. et al. Postoperative changes in
neutrophil-to-lymphocyte ratio and platelet
count: A simple prognostic predictor for adult-
to-adult living donor liver transplantation.
Asian J. Surg. 1–8 (2016). doi:10.1016/j.
asjsur.2017.02.004
8. Walker, P. A., Kunjuraman, B. & Bartolo,
D. C. C. Neutrophil-to-lymphocyte ratio
predicts anastomotic dehiscence. ANZ J.
Surg. (2018). doi:10.1111/ans.14369
9. Bustan, Y. et al. Elevated neutrophil to
lymphocyte ratio in non-affective psychotic
adolescent inpatients: Evidence for early
association between inflammation and
psychosis. Psychiatry Res.262, 149–153
(2018).
10. Paliogiannis, P. et al. Neutrophil to
lymphocyte ratio and clinical outcomes
in COPD: recent evidence and future
perspectives. Eur. Respir. Rev.27, 170113
(2018).
11. Wang, S. et al. Neutrophil-to-Lymphocyte
Ratio and Platelet-to-Lymphocyte Ratio Are
Effective Predictors of Prognosis in Patients with Acute Mesenteric Arterial Embolism
and Thrombosis. Annals of Vascular Surgery
(2018). doi:10.1016/j.avsg.2018.01.059
12. Argeny, S. et al. Prognostic value of
preoperative neutrophil-to-lymphocyte ratio
in Crohn’s disease. Wien. Klin. Wochenschr.
(2018). doi:10.1007/s00508-018-1322-3
13. Velissaris, D., Pantzaris, N.-D., Bountouris, P.
& Gogos, C. Correlation between neutrophil-
to-lymphocyte ratio and severity scores in
septic patients upon hospital admission. A
series of 50 patients. Rom. J. Intern. Med.0,
(2018).
14. Lee, J. W. et al. Prediction of renal cortical
defect and scar using neutrophil-to-
lymphocyte ratio in children with febrile
urinary tract infection. Nuklearmedizin56,
109–114 (2017).
15. Shin, H.-C. et al. Combined Use of Neutrophil
to Lymphocyte Ratio and C-Reactive Protein
Level to Predict Clinical Outcomes in Acute
Myocardial Infarction Patients Undergoing
Percutaneous Coronary Intervention. Korean
Circ. J.47, 383 (2017).
16. Joseph, J. T. & Jindal, R. M. Influence of
dialysis on post-transplant events. Clin.
Transplant.16, 18–23 (2002).
17. Gu, L. et al. Prognostic value of preoperative
inflammatory response biomarkers in patients
with sarcomatoid renal cell carcinoma and
the establishment of a nomogram. Sci. Rep.6,
1–10 (2016).
18. Tomita, M., Shimizu, T., Ayabe, T., Nakamura,
K. & Onitsuka, T. Elevated preoperative
inflammatory markers based on neutrophil-
to-lymphocyte ratio and C-reactive protein
predict poor survival in resected non-small
cell lung cancer. Anticancer Res.32, 3535–8
(2012).
19. Kurtul, A. et al. Association of platelet-
to-lymphocyte ratio with severity and
complexity of coronary artery disease in
patients with acute coronary syndromes. Am.
J. Cardiol.114, 972–8 (2014).
20. Oylumlu, M. M. et al. Platelet-to-lymphocyte
ratio is a predictor of in-hospital mortality
patients with acute coronary syndrome.
Anatol. J. Cardiol.15, 277–283 (2015).
21. Turkmen, K. et al. Platelet-to-lymphocyte
ratio better predicts inflammation than
neutrophil-to-lymphocyte ratio in end-stage
renal disease patients. Hemodial. Int.17,
391–396 (2013).
22. Yaprak, M. et al. Platelet-to-lymphocyte ratio
predicts mortality better than neutrophil-to-
lymphocyte ratio in hemodialysis patients.
Int. Urol. Nephrol.48, 1343–1348 (2016).
23. Ahbap, E. et al. Neutrophil-to-lymphocyte
ratio and platelet-tolymphocyte ratio in
evaluation of inflammation in end-stage renal
disease. Clin. Nephrol.85 (2016), 199–208
(2016).
24. Gabay, C. & Kushner, I. Acute-Phase
Proteins and Other Systemic Responses to
Inflammation. N. Engl. J. Med.340, 448–454
(1999).
25. Ioannou, A., Lucca, J. D. & Tsokos, G.
C. Immunopathogenesis of ischemia/
reperfusion-associated tissue damage.
Clinical Immunology141, 3–14 (2011).
26. Sieńko, J. et al. Role of platelets in the
modulation of kidney allograft recipients’
immune systems. Ann. Transplant.18, 76–81
(2013).
27. Salazar Meira, F. et al. Factors Associated With Delayed Graft Function and Their
Influence on Outcomes of Kidney
Transplantation. Transplant. Proc.48, 2267–
2271 (2016).
28. Gavela Martínez, E. et al. Delayed graft
function after renal transplantation: An
unresolved problem. Transplant. Proc.43,
2171–2173 (2011).
29. Tugmen, C. et al. Delayed Graft Function
in Kidney Transplantation:Risk Factors
and Impact on Early Graft Function. Prog.
Transplant.26, 172–177 (2016).
30. Miglinas, M., Supranaviciene, L., Mateikaite,
K., Skebas, K. & Kubiliene, A. Delayed
graft function: Risk factors and the effects of
early function and graft survival. Transplant.
Proc.45, 1363–1367 (2013).
31. Sert, I., Colak, H., Tugmen, C., Dogan, S. M.
& Karaca, C. The effect of cold ischemia time
on delayed graft function and acute rejection
in kidney transplantation. Saudi J Kidney Dis
Transpl25, 960–966 (2014).
32. Jushinskis, J. et al. Risk factors for the
development of delayed graft function in
deceased donor renal transplants. Transpl.
Proc41, 746–748 (2009).