Abstract
Background: Urethral discharge is a symptom of
urethritis. Common organisms causing urethral discharge
are Neisseria gonorrhea and Chlamydia trachomatis.
Cephalosporines, Macrolides and Tetracycline groups of
drugs are commonly used for the treatment.
Materials and Method: This was a prospective, cross
sectional, observational study. The patients were enrolled
from the Sexually Transmitted Infections clinic and also
from the hospital laboratory in between the period of one
year. All the male cases with urethral discharge at STI
clinic in between this period were included for clinical
examination and laboratory testing. All urine and discharge
specimens of urethral discharge patients as referred from
other departments directly to the hospital laboratory for
relevant tests were also included for the study.
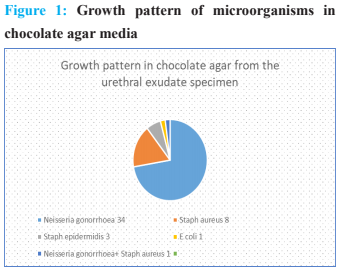
Results: Neisseria gonorrhea was the most common
agent of urethral discharge in male patients. Urethral
discharge, dysuria and inguinal lymphadenopathy were
common symptoms. All the NG isolates were sensitive to
Ceftriaxone and Imipenam.
Conclusion: Continuous monitoring with culture
sensitivity testing of urethral discharge cases is required.
References
Vigneswaran HT, Baird G, Hwang K, Renzulli
J, Chan PA. Etiology of symptomatic urethritis in
men and association with sexual behaviors. R I Med
J 2013. 2016 Jun 1;99(6):37–40.
Bachmann LH, Manhart LE, Martin DH, Seña
AC, Dimitrakoff J, Jensen JS, et al. Advances in the
Understanding and Treatment of Male Urethritis.
Clin Infect Dis. 2015 Dec 15;61(suppl_8):S763-9.
Gonococcal Infections - 2015 STD Treatment
Guidelines [Internet]. 2018 [cited 2018 Sep 18]. Available from: https://www.cdc.gov/std/tg2015/
gonorrhea.htm
World Health Organization, Reproductive
Health and Research. WHO guidelines for the
treatment of Neisseria gonorrhoeae. [Internet].
[cited 2018 Sep 18]. Available from: http://
www.ncbi.nlm.nih.gov/books/NBK379221/
Judson FN. Gonococcal Urethritis-Diagnosis
and Treatment. Arch Androl. 1979 Jan; 3(4):329–
Chernesky MA. The laboratory diagnosis of
Chlamydia trachomatis infections. Can J Infect Dis
Med Microbiol. 2005;16(1):39–44.
Keegan MB, Diedrich JT, Peipert JF. Chlamydia
trachomatis Infection: Screening and Management.
J Clin Outcomes Manag JCOM. 2014 Jan;21(1):30–
Nayak AK, Anoop TV, Sacchidanand S.
A clinico-etiological study of urethritis in men
attending sexually transmitted disease clinic at a
tertiary hospital. Indian J Sex Transm Dis AIDS.
;38(2):136–41.
Hill SA, Masters TL, Wachter J. Gonorrhea -
an evolving disease of the new millennium. Microb
Cell. 2016;3(9):371–389. Published 2016 Sep 5.
doi:10.15698/mic2016.09.524.
Gonorrhoea & its co-infection with other
ulcerative, non-ulcerative sexually transmitted &
HIV infection in a Regional STD Centre [Internet].
[cited 2019 Aug 27]. Available from: https://www.
ncbi.nlm.nih.gov/pmc/articles/PMC3103165/
Johnson RE, Newhall WJ, Papp JR, Knapp
JS, Black CM, Gift TL, et al. Screening tests
to detect Chlamydia trachomatis and Neisseria
gonorrhoeae infections--2002. MMWR Recomm
Rep Morb Mortal Wkly Rep Recomm Rep. 2002
Oct 18;51(RR-15):1–38; quiz CE1-4.
Lama L, Kayestha BMM. Gonococcal culture
and drug sensitivity pattern in patients with urethral discharge and vaginal discharge with cervicitis.
Post-Grad Med J NAMS [Internet]. 2017 Sep 7
[cited 2018 Aug 14];13(2). Available from: https://
pmjn.org.np/index.php/pmjn/article/view/222
Epidemiological Trends of Antibiotic Resistant
Gonorrhoea in the United Kingdom [Internet].
[cited 2019 Aug 27]. Available from: https://www.
ncbi.nlm.nih.gov/pmc/articles/PMC6165062/
Ohnishi M, Golparian D, Shimuta K, Saika T,
Hoshina S, Iwasaku K, et al. Is Neisseria gonorrhoeae
Initiating a Future Era of Untreatable Gonorrhea?:
Detailed Characterization of the First Strain with
High-Level Resistance to Ceftriaxone. Antimicrob
Agents Chemother. 2011 Jul;55(7):3538–45.
Buder S, Dudareva S, Jansen K, Loenenbach A,
Nikisins S, Sailer A, et al. Antimicrobial resistance
of Neisseria gonorrhoeae in Germany: low levels
of cephalosporin resistance, but high azithromycin
resistance. BMC Infect Dis. 2018 17;18(1):44.
Lee RS, Seemann T, Heffernan H, Kwong JC,
Gonçalves da Silva A, Carter GP, et al. Genomic
epidemiology and antimicrobial resistance
of Neisseria gonorrhoeae in New Zealand. J
Antimicrob Chemother. 2018 Feb 1;73(2):353-64.
Kulkarni SV, Bala M, Muqeeth SA, Sasikala
G, Nirmalkar AP, Thorat R, et al. Antibiotic
susceptibility pattern of Neisseria gonorrhoeae
strains isolated from five cities in India during
-2016. J Med Microbiol. 2018 Jan;67(1):22–8.
Wi T, Lahra MM, Ndowa F, Bala M, Dillon
J-AR, Ramon-Pardo P, et al. Antimicrobial resistance
in Neisseria gonorrhoeae: Global surveillance
and a call for international collaborative action.
PLoS Med [Internet]. 2017 Jul 7 [cited 2019 Aug
;14(7). Available from: https://www.ncbi.nlm.
nih.gov/pmc/articles/PMC5501266/