Abstract
Introduction: Iron deficiency anemia (IDA) is the most common anemia
worldwide. It adversely affects the physical growth, cognition, behavior and the
immune status of infants and children. There are limited number of studies
in Nepal analyzing its prevalence, risk factors and diagnosis in pediatric
population. Restriction of analgesics intake, increased intake of iron rich food
and deworming are important determinants in the disease management.
Methods: Hospital based prospective comparative study was conducted
in the Department of Pediatrics in Manipal Teaching Hospital from December
2014 to December 2016 enrolling all children aged 6 months to 5 years with
anemia. Demographic profile, clinical features and information regarding risk
factors were noted along with detailed physical examination. Iron profile was
done to confirm diagnosis of IDA. Data was analyzed using SPSS 21.
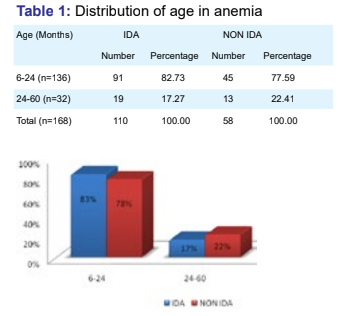
Results: Out of 168 anemic children, 110 (65.45%) children were diagnosed
as IDA. Dietary factors, pica and intake of analgesics/antipyretics were major
risk factors. Serum iron, serum ferritin, transferrin saturation were low whereas
total iron binding capacity was high in IDA.
Conclusion: Iron deficiency anemia is a common, preventable and easily
treatable disease which has potentially serious consequences if not treated.
Non compliance to exclusive breastfeeding in the first 6 months of life,
introduction of cow’s/buffalo’s milk in the first year, pica and rampant use of
analgesics/antipyretics are major risk factors.
References
2. World Health Organisation. The World Health Report 2002: Reducing Risks, Promoting Healthy Life. Geneva: World Health Organisation;
2002. [cited 2014 May 30]. Available from: www.who.int/whr/2002/en/whr02_en.pdf.
3. Department of Health Services. Ministry of Health and Population. Annual report. 2069/70 (2012/2013):21.
4. Lozoff B. Iron deficiency and child development. Food Nutr Bull 2007;28(4):560–571.
5. Iannotti LL, Tielsch JM, Black MM, Black RE. Iron supplementation in early childhood: health benefits and risks. Am J Clin Nutr
2006;84(6):1261–1276.
6. Johnson-Wimbley TD, Graham DY. Diagnosis and management of iron deficiency anemia in the 21st century. Therap Adv Gastroenterol
2011;4(3):177-184.
7. Stoltzfus RJ. Iron deficiency: global prevalence and consequences. Food Nutr Bull 2003;24: S99.
8. Sills R. Iron Deficiency Anemia. In: Kliegman R. Nelson textbook of Pediatrics. 20th ed. Philadelphia:Elsevier/Saunders;
2016.p.2323-2326.
9. Aulakh R, Sohi I, Singh T, Kakkar N. Red cell distribution width (RDW) in the diagnosis of iron deficiency with microcytic hypochromic
anemia. Indian J Pediatr 2009;76(3):265-268.
10. Gupta SK, Bansal D, Malhi P, Das R. Developmental profile in children with iron deficiency anemia and its changes after therapeutic iron
supplementation. Indian J Pediatr 2010;77(4):375-379.
11. Sazawal S, Dhingra U, Dhingra P, Dutta A, Shabir H. Efficiency of red cell distribution width in identification of children aged 1-3 years
with iron deficiency anemia against traditional hematological markers. BMC Pediatr 2014;14:18.
12. Munoz JA, Marcos J, Risueno CE. Déficit de hierro y pica. Sangre (Barc) 1998;43:31–34.
13. Ziegler EE, Fomon SJ, Nelson SE. Cow milk feeding in infancy: further observations on blood loss from the gastrointestinal tract. J
Pediatr 1990; 116:11.
14. Gaskell H, Derry S, Moore RA. Is there an association between low dose aspirin and anemia (without overt bleeding)? Narrative review.
BMC Geriatr 2010;10:71.
15. Rockey DC, Cello JP. Evaluation of the gastro-intestinal tract in patients with iron-deficiency anemia. N Engl J Med 1993;329:1691–
1695.
16. Cook, IJ, Pavli P, Riley JW, Goulston KJ, Dent OF. Gastrointestinal investigation of iron deficiency anemia. BMJ 1986;292:1380–1382.
17. Montresor A, Albonico M, Khalfan N, Stoltzfus RJ, Tielsch JM, Chwaya HM, et al. Field trial of a hemeoglobin colour scale: an effective
tool to detect anemia in preschool children. Tropical Medicine & International Health 2000;5(2):129-133.
18. Stoltzfus RJ, Edward-Raj A, Dreyfuss ML, Albonico M, Montresor A, Thapa MD, et al. Clinical pallor is useful to detect severe anemia in
populations where anemia is prevalent and severe. J Nutr 1999;129(9):1675-1681.
19. Bainton DF, Ullyot JL, Farquhar MG. The development of neutrophilic polymorphonuclear leukocytes in human bone marrow. The
Journal of Experimental Medicine. 1971;134(4):907–934
20. Brittenham GM. Disorders of iron metabolism: iron deficiency and overload. Hematology: Basic Principles And Practice. 2000;3:397–
428.
21. Mohammed Mujib AS, Mohammad Mahmud AS, Halder M, Monirul Hasan CM. Study of Hematological Parameters in Children Suffering
from Iron Deficiency Anemia in Chattagram Maa-o-Shishu General Hospital, Chittagong, Bangladesh. Anemia. 2014;2014:503981.