Abstract
Introduction: Perinatal asphyxia is one of the leading
causes of neonatal death in developing countries like
Nepal. This study was done to evaluate the prevalence,
risk factors and immediate outcome of perinatal
asphyxia in newborns.
Materials and Methods:This was a prospective, cross
sectional, observational study conducted in Neonatal
Intensive Care Unit of Pokhara Academy of Health
Sciences during a period of six months including
60 neonates. All inborn neonates with diagnosis of
perinatal asphyxia with neonatal encephalopathy
were included in the study and Hypoxic Ischemic
Encephalopathy (HIE) staging was done. The
important maternal risk factors and fetal risk factors
and immediate outcome of neonates were recorded.
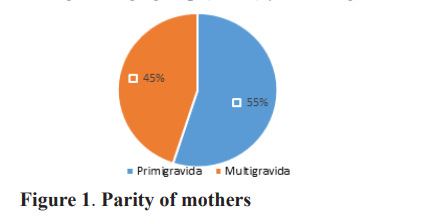
Results: The prevalence of perinatal asphyxia was
14.5 per 1000 live births; males 45% (27) and females
55% (33). Meconium-stained liquor was the most
common risk factor accounting for 36.7% of cases
followed by premature rupture of membrane (26.7%),
maternal fever (6.7%). HIE III had (100%) mortality
followed by HIE II (15.3%) and HIE I (5.1%)
respectively whereas HIE stage I had good recovery
(94.8%) followed by HIE II (84.6%).
Conclusion: Meconium-stained amniotic fluid and
premature rupture of membrane are the two most
common risk factors. Early detection and timely
intervention of high-risk factors causing perinatal
asphyxia can decrease mortality as well as morbidity.
References
Resuscitation; A Practical Guide. World
Health Organization: Geneva 1997 [ Accessed
February 27,2007.Available:http:www.who.int/
reproductive health/publication/MSM 98
/introduction en.html.
2. Neonatal Encephalopathy and Neurologic
Outcome, Second EditionReport of
the American College of Obstetricians
and Gynecologists’ Task Force on
Neonatal Encephalopathy | American
Academy of Pediatrics
[Internet]. [cited 2021 May 25].
Available from: https://pediatrics.
aappublications.org/content/133/5/e1482
3. Black RE, Cousens S, Johnson HL, Lawn JE,
Rudan I, Bassani DG, et al. Global, regional,
and national causes of child mortality in 2008: a
systematic analysis. Lancet Lond Engl. 2010
Jun 5;375(9730):1969–87.
4. Sankar MJ, Natarajan CK, Das RR, Agarwal R,
Chandrasekaran A, Paul VK. When do newborns
die? A systematic review of timing of overall and
cause-specific neonatal deaths in developing
countries. J Perinatol. 2016;36(1):S1–11.
5. Velaphi S, Pattinson R. Avoidable factors and
causes of neonatal deaths from perinatal
asphyxia-hypoxia in South Africa: national
perinatal survey. Ann Trop Paediatr. 2007 Jun
1;27(2):99–106.
6. Sarnat HB, Sarnat MS. Neonatal encephalopathy
following fetal distress. A clinical and
electroencephalographic study. Arch Neurol.
1976 Oct;33(10):696–705.
~443~˷
Original Article Medical Journal of Pokhara Academy of Health Sciences Vol 5 Issue 1 Jan-Jun 2022
7. Cameron W,thomas. Hypoxic- Ischemic
Encephalopathy. In: Nelson Text book of
Pediatrics. 2021. p. 3944–5.
8. Tabassum F, Rizvi A, Ariff S, Soofi S, Bhutta
ZA. Risk Factors Associated with Birth
Asphyxia in Rural District Matiari, Pakistan: A
Case Control Study. Int J Clin Med. 2014 Dec
4;5(21):1430–41.
9. Souza ALS de, Souza NL de, França DF
de, Oliveira SIM de, Araújo AKC, Dantas
DNA. Risk Factors for Perinatal Asphyxia in
Newborns Delivered at Term. Open J Nurs.
2016 Jul 8;6(7):558–64.
10. Tasew H, Zemicheal M, Teklay G, Mariye T,
Ayele E. Risk factors of birth asphyxia among
newborns in public hospitals of Central Zone,
Tigray, Ethiopia 2018. BMC Res Notes. 2018
Jul 20;11(1):496.
11. Manandhar SR, Basnet R. Prevalence of
perinatal asphyxia in neonates at a tertiary
care hospital: a descriptive cross-sectional
study. JNMA: Journal of the Nepal Medical
Association. 2019 Sep;57(219):287.
12. Rainaldi MA, Perlman JM. Pathophysiology
of Birth Asphyxia. Clin Perinatol. 2016 Sep
1;43(3):409–22.
13. Lives SN. State of the World’s Newborns.
Wash DC Save Child. 2001;
14. Shrestha S, Shrestha GS, Sharma A.
Immediate Outcome of Hypoxic Ischaemic
Encephalopathy in Hypoxiate Newborns in
Nepal Medical College. J Nepal Health Res
Counc. 2016 May 1;14(33):77–80.
15. Dongol S, Singh J, Shrestha S, Shakya A.
Clinical Profile of Birth Asphyxia in Dhulikhel
Hospital: A Retrospective Study. J Nepal
Paediatr Soc. 2010;30(3):141–6.
16. Lee ACC, Mullany LC, Tielsch JM, Katz J,
Khatry SK, LeClerq SC, et al. Risk Factors for
Neonatal Mortality Due to Birth Asphyxia in
Southern Nepal: A Prospective, CommunityBased Cohort Study. Pediatrics. 2008 May
1;121(5):e1381–90.
17. Hillier SL, Witkin SS, Krohn MA, Watts DH,
Kiviat NB, Eschenbach DA. The relationship
of amniotic fluid cytokines and preterm
delivery, amniotic fluid infection, histologic
chorioamnionitis, and chorioamnion infection.
Obstet Gynecol. 1993 Jun;81(6):941–8.
18. Aslam HM, Saleem S, Afzal R, Iqbal U, Saleem
SM, Shaikh MWA, et al. “Risk factors of birth
asphyxia.” Ital J Pediatr. 2014 Dec 20;40(1):94.
19. Baker PN, Kenny L. Obstetrics by Ten
Teachers, 19th Edition. CRC Press; 2011. 338
p.
20. Padayachee N, Ballot DE. Outcomes of
neonates with perinatal asphyxia at a tertiary
academic hospital in Johannesburg, South
Africa. South Afr J Child Health. 2013 Sep
6;7(3):89–94.
21. Yadav N, Damke S. Study of risk factors
in children with birth asphyxia. Int J
ContempPediatr. 2017 Feb 22;4:518.
22. Palsdottir K, Dagbjartsson A, Thorkelsson T,
Hardardottir H. [Birth asphyxia and hypoxic
ischemic encephalopathy, incidence and
obstetric risk factors]. Laeknabladid. 2007 Sep
1;93(9):595–601.
23. Wiswell TE, Gannon CM, Jacob J, Goldsmith
L, Szyld E, Weiss K, et al. Delivery room
management of the apparently vigorous
meconium-stained neonate: results of the
multicenter, international collaborative trial.
Pediatrics. 2000 Jan;105(1 Pt 1):1–7.
24. Azam M, Malik F, Khan P. Birth asphyxia;
risk factors | Virtual Health Sciences Library
[Internet]. 2020 [cited 2022 Apr 2]. Available
from: https://vlibrary.emro.who.int/imemr/
birth-asphyxia-risk-factors/
25. Finer NN, Robertson CM, Richards RT,
Pinnell LE, Peters KL. Hypoxic-ischemic
encephalopathy in term neonates: Perinatal
factors and outcome. J Pediatr. 1981 Jan
1;98(1):112–7.
26. Robertson C, Finer N. Term Infants with
Hypoxic-Ischemic Encephalopathy: Outcome
at 3.5 Years. Dev Med Child Neurol.
1985;27(4):473–84.
27. Shankaran S, Woldt E, Koepke T, Bedard MP,
Nandyal R. Acute neonatal morbidity and
long-term central nervous system sequelae of
perinatal asphyxia in term infants. Early Hum
Dev. 1991 May 1;25(2):135–48.