Abstract
Introduction: Acute tonsillitis is a common
problem in patients who present to the Ear, Nose,
Throat Out Paitent Department (ENT OPD).
Children and young adults are commonly affected.
Antibiotics are generally prescribed in such patients
empirically. This study aims to find out the common
agents causing acute tonsillitis and clinical response
to oral Cloxacillin.
Materials and methods: This is a cross sectional
observational study conducted from July 2018
to June 2019 in the Department of ENT, Pokhara
Academy of Health Sciences, Pokhara. Throat swab
was sent for culture and patients were prescribed
oral Cloxacillin. Patients were analyzed after
culture sensitivity reports for improvement of their
symptoms on 5th to 6th day of treatment. McIsaac
score less than 3 was considered as treated and
score >3 considered untreated.
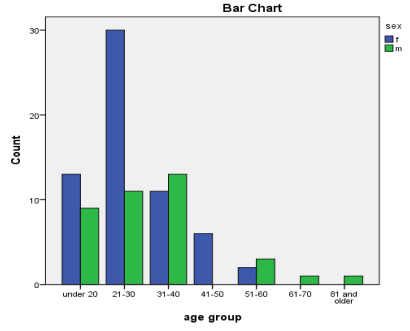
Results: Acute tonsillitis was the most frequent in
age group 21-30 years and group A Beta hemolytic
streptococcus was the most common isolate.
Cloxacillin is found to be effective in the treatment
of acute bacterial tonsillitis.
Conclusion: This study suggests that oral Cloxacillin
is effective in treatment of acute tonsillitis & the
most common organism isolated was B Hemolytic
streptococcus.
References
Comparative study of bacteriology in recurrent
tonsillitis among children and adults. Singapore
medical journal. 2006 Apr 1;47(4):271.
2. Shrestha R, Karki S, Manandhar T, Deo S.
Comparative study on efficacyof amoxicillin
with clavulanic acid versus azithromycin in
tonsillitis. J Univ CollMed Sci. 2018 Nov
20;6(1):22–6.
3. Sigdel B, Dubey T, Nepali R, Kc N. Prescription
patterns of Antibiotics inAcute tonsillitis:
Hospital-based study. J Gandaki Med Coll
Nepal. 2020 Jun18;13(1):65–7.
4. John LJ, Cherian M, Sreedharan J, Cherian
T. Patterns of Antimicrobialtherapy in acute
tonsillitis: A cross-sectional Hospital-based
study from UAE.AnAcad Bras Ciênc. 2014
Mar;86(1):451–7.
5. Cavalcanti VP, Camargo LA de, Moura FS,
Fernandes EJ de M, Lamaro-Cardoso J, Braga
CA da SB, et al. Staphylococcus aureus in
tonsils of patientswith recurrent tonsillitis:
prevalence, susceptibility profile, and
genotypiccharacterization. The Brazilian Journal
of Infectious Diseases. 2019 Jan;23(1):8–
6. Vasudevan J, Mannu A, Ganavi G. McIsaac
modification of centor score in diagnosis
of streptococcal pharyngitis and antibiotic
sensitivity pattern of beta-hemolytic streptococci
in Chennai, India. Indian pediatrics. 2019 Jan
1;56(1):49-52.
7. Stuck BA, Windfuhr JP, Genzwurker H, Schroten
H, Tenenbaum T, Gotte K. Tonsillectomy in
children. DtschArztebl Int. 2008;105:852–61
8. Khadilkar MN, Ankle NR. Anaerobic
bacteriological microbiota in surface and core
of tonsils in chronic tonsillitis. J Clin Diagn
Res. 2016;10:MC01–3.
9. Darod HH, Melese A, Kibret M, Mulu
W. Bacterial Tonsillitis and Antimicrobial
Resistance Profiles Among Children Within
Five Years of Age At Hargeisa Group of
Hospital, Somaliland: A Cross-Sectional Study.
10. Shankar PR, Upadhyay DK, Subish P, Dubey
AK, Mishra P. Prescribing patterns among
pediatric inpatients in a teaching hospital in
western Nepal. Singapore Med J 2006;47:261-
5).
11. Sigdel B. The Shift of Bacterial Sensitivity
with Antibiotics in Acute Tonsillitis. Journal of
Nobel Medical College. 2021 Jun 16;10(1):3-6.
12. Ylikoski J, Karjalainen J. Acute tonsillitis
in young men: etiological agents and their
differentiation. Scandinavian journal of
infectious diseases. 1989 Jan 1;21(2):169-74.
13. Putto A. Febrile exudative tonsillitis: viral or
streptococcal?. Pediatrics. 1987 Jul;80(1):6-12.
14. Ain MR, Shahzad N, Aqil M, Alam MS, Khanam
R. Drug utilization pattern of antibacterials
used in ear, nose and throat outpatient and
inpatient departments of a university hospital at
New Delhi, India. J Pharm Bioallied Sci. 2010
Jan;2(1):8-12. doi: 10.4103/0975-7406.62695.
21814423; PMCID: PMC3146095.
15. Suaifan GA, Shehadeh M, Darwish DA, Al-Ije
H, Yousef AM, Darwish RM. A cross-sectional
study on knowledge, attitude and behavior
related to antibiotic use and resistance among
medical and non-medical university students
in Jordan. African Journal of Pharmacy and
Pharmacology. 2012 Mar 15;6(10):763-70.