Abstract
Introduction:- Neonatal jaundice is one of the
most frequently encountered clinical problems in
newborns. Early intervention is needed to prevent
complications caused by increased level of serum
bilirubin. Kramer’s method is a non invasive visual
assessment technique to estimate the bilirubin
levels in neonates with jaundice especially useful
in low income settings like Nepal. This study was
conducted to determine whether visual assessment
of neonatal jaundice could serve as a screening
step for neonatal hyperbilirubinemia and this type
of non-invasive measurement of neonatal jaundice
has not been done in our settings.
Materials and Methods:- A prospective cross
sectional study was performed over a period of 12
months at Emergency Ward, Neonatal Intermediate
Care Unit (NIMCU), Neonatal Intensive Care unit
(NICU) of Kanti Children’s Hospital, Maharajgunj
Kathmandu where term neonates with jaundice
were assessed visually for jaundice by a single
pediatrician and categorized into different dermal
zones according to Kramer’s rule and mean of
three observations was taken as visual estimation of
jaundice and compared with total serum bilirubin
levels.
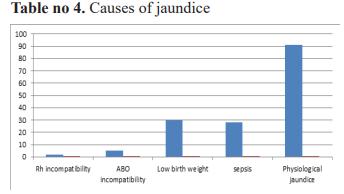
Results:- The common causes of neonatal jaundice
were physiological jaundice (56.17%) low birth
weight (18.5%) and sepsis (17.3%). The visual
assessment of neonatal jaundice was highly
correlated with total serum bilirubin level (Pearson's
correlation coefficient=0.837 with p value <0.0001).
Conclusion:Visual assessment of neonatal jaundice by Kramers’s rule was highly correlated with total serum bilirubin level. So, it can be used as a screening tool for
predicting neonatal hyperbilirubinemia
References
Gregory M CJ Manual of neonatal care 6th ed
New Delhi: Wolters Kluwer; 2011 304-39 p.
2. Erin E,Kliegman RM, Behrman RE, Jenson HB,
Stanton BM. Jaundice and hyperbilirubinemia
in neonate. In: Nelson textbook of pediatrics
e-book. 21st ed. Elsevier Health Sciences; p.
4097–113.
3. Bichha RP. A Glimpse of Neonatal Intermediate
Care Unit (NIMCU) in Year 2071. 53rd
Anniversery of Kanti Children Hospital 2071
Souvenir. 2071:15 to 7. In.
4. Gupta A, Kumar A, Khera P. Method and model
for Jaundice prediction through non-invasive
Bilirubin detection technique. Int J Eng Res
Comparison of Visual Assessment of Neonatal Jaundice. Ghimire S et. al.
~414~˷
Original Article Medical Journal of Pokhara Academy of Health Sciences Vol. 4 Issue 2 July-December 2021
Technol IJERT. 2015;4(8):34–8.
5. Kramer LI. Advancement of dermal icterus
in the jaundiced newborn. Am J Dis Child.
1969;118(3):454–8.
6. Ebbesen F. The relationship between the
cephalo-pedal progress of clinical icterus and
the serum bilirubin concentration in newborn
infants without blood type sensitization. Acta
Obstet Gynecol Scand. 1975;54(4):329–32.
7. Das S, van Landeghem FKH. Clinicopathological
Spectrum of Bilirubin Encephalopathy/
Kernicterus. Diagnostics [Internet]. 2019 Feb
28 [cited 2021 Jun 8];9(1). Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/
PMC6468386/
8. Subcommittee on Hyperbilirubinemia.
Management of Hyperbilirubinemia in the
Newborn Infant 35 or More Weeks of Gestation.
PEDIATRICS [Internet]. 2004 Jul 1 [cited 2021
Jun 7];114(1):297–316. Available from: http://
pediatrics.aappublications.org/cgi/doi/10.1542/
peds.114.1.297
9. Dhanjal GS, Jain G, Singh M. Clinicoetiological study of neonatal jaundice in a
tertiary carecentre in Ambala (Haryana) India.
JBPR. 2014;3(1):64–7.
10. Kaini NR, Chaudhary D, Adhikary V,
Bhattacharya S, Lamsal M. Overview of
cases and prevalence of jaundice in neonatal
intensive care unit. Nepal Med Coll J NMCJ.
2006;8(2):133–5.
11. Koosha A, Rafizadeh B. Evaluation of neonatal
indirect hyperbilirubinaemia at Zanjan Province
of Iran in 2001-2003: prevalence of glucose-6-
phosphate dehydrogenase deficiency. Singapore
Med J. 2007;48(5):424.
12. Tiker F, Tarcan A, Kilicdag H, Gurakan B.
Early onset conjugated hyperbilirubinemia
in newborn infants. Indian J Pediatr. 2006
May;73(5):409–12.
13. Pediatrics AA of. Provisional Committee
for Quality Improvement and Subcommittee
on Hyperbilirubinemia. Practice parameter:
management of hyperbilirubinemia in the healthy
term newborn. Pediatrics. 1994;94(4):558–65.
14. Huang M-S, Lin M-C, Chen H-H, Chien K-L,
Chen C-H. Risk factor analysis for late-onset
neonatal hyperbilirubinemia in Taiwanese
infants. Pediatr Neonatol. 2009;50(6):261–5.
15. Najib KS, Saki F, Hemmati F, Inaloo S.
Incidence, risk factors and causes of severe
neonatal hyperbilirubinemia in the South of
iran (fars province). Iran Red Crescent Med J.
2013;15(3):260.
16. Newman TB, Xiong B, Gonzales VM, Escobar
GJ. Prediction and prevention of extreme
neonatal hyperbilirubinemia in a mature health
maintenance organization. Arch Pediatr Adolesc
Med. 2000;154(11):1140–7.
17. Riskin A, Tamir A, Kugelman A, Hemo M,
Bader D. Is visual assessment of jaundice
reliable as a screening tool to detect significant
neonatal hyperbilirubinemia? J Pediatr.
2008;152(6):782–7.
18. Madlon-Kay DJ. Home health nurse clinical
assessment of neonatal jaundice: comparison
of 3 methods. Arch Pediatr Adolesc Med.
2001;155(5):583–6.