Abstract
Introduction: Exclusive breastfeeding practice for
six months of life is very effective intervention for
reducing childhood morbidity and mortality and to
prevent different forms of childhood malnutrition.
But, adherence to exclusive breastfeeding is difficult.
Family support after delivery is also very important
for the quality life of both mother and baby.
Materials and Methods: This was a cross-sectional
study conducted in two different hospitals in Pokhara,
Western Nepal from July 2017 to July 2018. 1050
mothers who came for hospital visit were interviewed
regarding their breast-feeding and complimentary
feeding practice
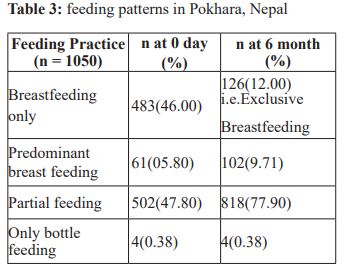
Results: During the antenatal visit 86.85%received
information on breastfeeding while only 5.14%
mothers were given information about the importance
of colostrum and 64.57% initiated breastfeeding
within one hour of delivery. Exclusive breastfeeding
at 0 day was 46%, predominant breast feeding was
5.8% and partial feeding was 47.8% respectively.
Four mothers (0.38%) refused to feed breast milk. The
association between sex of child and support pattern of
relatives during OPD checkup among Aryan families
was statistically significant in male child than female
child.
Conclusions: Exclusive breast feeding for six
months is advisable but few mothers practiced this.
Although pregnant women were given information
regarding breastfeeding during the antenatal visit,
very few knew the importance of colostrum, so proper
counseling during antenatal visit is necessary. Social
support by the husband and his relatives should be
done especially when female child is born.
References
Hunger. Malnutrition and the First 1,000 Days of
Life: Causes, Consequences and Solutions. World
Rev Nutr Diet. Basel, Karger, 2016, vol115,pp82-97.
(DOI:10.1159/000442075)
2. WHO: The optimal duration of exclusive
breast feeding: reports of an expert consultation
Geneva, WHO; 2001.
3. De Onis M, Garza C, Onyango AW,
Rolland-Cachera MF: [WHO growthstandards for
infants and young children]. Arch Pediatr 2009,
16(1):47-53.
4. Haider R, Ashworth A, Kabir I, Huttly
SR: Effect of community-based peercounsellors
on exclusive breastfeeding practices in Dhaka,
Bangladesh: arandomised controlled trial. Lancet
2000, 356(9242):1643-1647.
5. Subba SH, TS Chandrashekhar, Binu VS,
Joshi HS, RanaMS : Infant feeding practices of
mothers in an urban area in Nepal. Kathmandu
University Medical Journal 2007, 5(1), :42-47.
6. Ministry of Health and Population
(MOHP), Nepal, NEW ERA and Macro
International Inc: Nepal Demographic Health
Survey 2016 Kathmandu, Nepal: Ministry of
Health and population, New ERA, and Macro
International Inc; 2017.
7. World Health Organization (WHO), WHO:
Indicators for Assessing Infant and Young Child
Feeding Practices [Internet]. Geneva. WHO; 2007.
Available from: http://apps.who.int/iris/bitstream/
handle/10665/43895/9789241596664_eng.pdf.
8. World Health Organization (WHO), WHO
statement on Caesarean section rates [Internet].
Geneva.WHO;2015.Availablefrom: http://apps.
who.int/iris/bitstream/10665/161442/1/WHO_
RHR_15.02_eng.pd
9. Chandrashekhar TS, Joshi HS, Binu V,
Shankar PR, Rana MS, Ramachandran U: Breastfeeding initiation and determinants of exclusive
breast-feeding - a questionnaire survey in an urban
population of western Nepal. Public Health Nutr
2007, 10(2):192-197.
10. Aryal TR: Breastfeeding in Nepal: patterns
and determinants. JNMA J Nepal Med Assoc 2007,
46(165):13-19.
11. Cheng CY, Pickler RH. Effects of stress and
social support on postpartum health of Chinese
mothers in the United States. Res Nurs Health.
2009; 32(6):582–591. [PubMed: 19877163]
12. Cutrona CE, Troutman BR. Social support,
infant temperament, and parenting self-efficacy:
a mediational model of postpartum depression.
Child Dev. 1986; 57(6):1507–1518. [PubMed:
3802975]
13. Rennie Negron, Anika Martin,
MeitalAlmog et al: Social support during the
postpartum period: Mothers’ views on needs,
expectations, and mobilization of support. Matern
Child Health J. 2013 May ; 17(4): 616–623.(
DOI:10.1007/s10995-012-1037-4)
14. O’Hara MW, Rehm LP, Campbell SB.
Postpartum depression: A role for social network
and life stress variables. J NervMent Dis. 1983;
171(6):336–341. [PubMed: 6854298]