Abstract
Introduction: Hyperbaric Bupivacaine is the most widely
used local anesthetic. A number of adjuvants have been used
with local anesthetic agents in order to improve the quality
and duration of analgesia and anesthesia. This study was
carried out to assess the efficacy of intrathecal Tramadol as
a spinal adjunct to prolong the duration of spinal anesthesia
in lower abdominal surgeries.
Materials and Methods: Sixty patients aged between
18 to 80 years, were randomly divided into two groups -
Tramadol and Placebo group. Spinal anesthesia was given
by using 25 Gauge Quinke spinal needle in sitting position
with midline approach. Patients belonging to Tramadol
group received 3 ml of 0.5% Bupivacaine along with 0.5
ml of Tramadol (25mg) and patients belonging to Placebo
group received 3 ml of 0.5% Bupivacaine along with 0.5
ml of Normal Saline. In the postoperative ward, duration
of analgesia was assessed by the time when first rescue
analgesia was given. Visual Analogue Scale for pain was
noted at the time of rescue analgesia. The total amount of
opioid consumed over 24 hour postoperative period was
noted. Hemodynamic like heart rate, systolic, diastolic and
mean arterial blood pressures were also noted. Data were
analyzed using independent t-test for continuous variables
and chi-square test for categorical variables, p value <0.05
was considered significant.
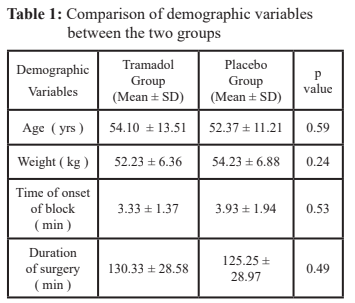
Results: The two groups were comparable with respect to
age, weight, sex, ASA grading and duration of surgery. Mean
duration of effective analgesia was 231.53 ± 22.00 min in
Tramadol group and 125.40 ± 8.86 min in Placebo group
(p = 0.001). The mean total amount of opioid consumption
in 24 hours postoperative period was 145.00 ± 30.31 mg
in Tramadol group and 171.67 ± 36.39 mg in Placebo
group (p = 0.003). Mean of Heart rate, systolic, diastolic
and mean arterial blood pressures were not significant
between the two groups. Incidence of nausea and vomiting
was statistically significant between the two groups with
a p value of 0.010. Hypotension and bradycardia was
statistically not significant between the two groups.
Conclusion:Tramadol was effective adjuvant to hyperbaric
bupivacaine for intrathecal use to increase the duration of
spinal anesthesia in patients undergoing lower abdominal
surgeries.
References
Fanelli G. Spinal anesthesia: an evergreen
technique. Acta Biomed 2008,79: 9-17.
2. Kleinman W, Mikhail M. Regional anesthesia
and pain management: spinal, epidural and
caudal blocks. In Morgan GE, Mikhail M,
Murray M, clinical anesthesiology 4th ed.
Singapore: McGraw Hill, 2008:290-291.
3. Brown DL. Spinal block in Atlas of Regional
Anesthesia, 2nd Edition, Philadelphia, WB
Saunders Company, 1999.
4. Yaksh T, Rudy T. Analgesia mediated by
a direct spinal action of narcotics. Science
1976; 192:1357-8.
5. Saxena AK, Arava SK. Current concepts in
Neuraxial administration of opiods and non
opiods: An overview and future perspectives.
Indian J Anaesth 2004;48(1):13-24.
6. Gustafsson LL, Schildt B, Jackobson K.
Adverse effects of extradural and intrathecal
opiates: Report of a nationwide survey in
Sweden. Br J Anaesth 1982;54:479-86.
7. Eisenach JC. Overview: First international
symposium on α2 adrenergic mechanism
of spinal anaesthesia. Regional Anaesth
1993;18(4s):i-iv.
8. Raffa RB, Friderichs E, Reimann W,
Shank RP, Codd EE, Vaught JL. Opioid
and non-opioid components independently
contribute to the mechanism of action of
tramadol, an `atypical’ opioid analgesic. J
Pharmacol Exp Ther. 1992; 260: 275-85.
9. Gunaydin B, Gungor I, Izdes S. Final
Baricity of Ropivacaine or Bupivacaine
combined with Fentanyl for Intrathecal
Administration. Turk J Med Science. 2012;
42(5): 942-45.
10. Chakraborty S, Chakraborty J, Bhattacharya
D. Intrathecal Tramadol Added to
Bupivacaine As Spinal Anesthetic Increases
Analgesics Effect Of The Spinal Blockade
After Major Gynaecological Surgeries.
Indian J Pharmacol. 2008; 40: (4): 180-2.
11. Mankeshwar HJ, Ganesh S. Preemptive
analgesia with intrathecal narcotic
(tramadol) for postoperative analgesia:
Journal clinical epidiomology. 1997; 50(1):
7S.
12. Mustafa G.M., Mohammad F.M. and
Waheed S.H.F. Which has greater analgesic
effect: Intrathecal Nalbuphina or Tramadol?
Journal of American Science. 2011; 7(7):
480-4.
13. Khoon A, Ahameed S, Shagafta Q.
Comparative study of intrathecal tramadol
administration on post operative analgesia
after transurethral resection of prostate
using three different doses of tramadol. http:
// dspasces. Uok.edu. in / jspui/ handle/ i/
887.
14. Alhasheimm JA, Kaki AM. Effect of
intrathecal tramadol administration on
postoperative pain after transurethral
resection of prostate. British J Anesthesia.
2003; 91: 536-40.
15. Malik A I, Sheikh I A, Qasmi S A, Ahmed A.
Comparison of tramadol with bupivacaine
as local anesthetics as post operative pain
control . Journal of Surgery of Pakistan.
2011; 16 (1): 10-13.