Abstract
Background: Inguinal hernia is one of the most
common surgical conditions in children. Herniotomy
is the surgery performed for a pediatric hernia
and hydrocele. This study was done to know the
demography and outcome of pediatric herniotomy
at our center.
Materials and methods: A prospective study on
patients who underwent herniotomy from 10th
May 2016 to 9th May 2017 was conducted at the
Department of Surgery, Western Regional Hospital.
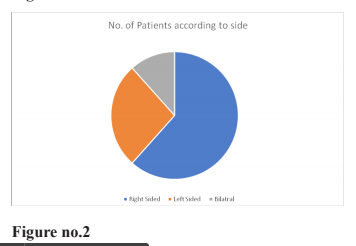
Results: During this study 112 patients underwent
herniotomy out of which 98 were boys while 14
were girls. 59(52.67%) patients had unilateral
hernia, 40(35.71%) had unilateral hydrocele and
13(11.6%) had bilateral condition among which 8
had hernia and 5 had hydrocele. 69(61.6%) patients
presented with a right-sided, 30(26.7%) with left-
sided, and 13(11.6%) with bilateral conditions.
13 patients (11.6%) presented at the emergency
with irreducible hernia. Two among the patient
who underwent emergency herniotomy developed
postoperative wound infection and one among the
elective surgery had recurrence.
Conclusion: Pediatric inguinal hernias and
hydroceles are often difficult to diagnose clinically.
Herniotomy is often performed by junior consultants
who have no specific training in pediatric surgery.
Timely planning of surgery is required to minimize
preoperative complications.
References
King SK. Jones’ clinical paediatric surgery. 7th edn.
Chichester: John Wiley & Sons, 2015. p. 332.
2. Clarke S. Pediatric inguinal hernia and hydrocele:
an evidence-based review in the era of minimal
access surgery. J Laparoendosc Adv Surg Tech A.
2010;20(3):305–9.
3. Nazem M, Heydari Dastgerdi MM, Sirousfard M.
Outcomes of pediatric inguinal hernia repair with or
without opening the external oblique muscle fascia.
Vol. 20, Journal of Research in Medical Sciences.
2015. p. 1172–6.
4. Coran AG, Fonkalsrud EW, Grosfeld JL, O’Neill
JA. 6th ed. Philadelphia: Mosby Elsevier; 2006.
Pediatric Surgery.
5. Yeap E, Nataraja RM, Pacilli M. Inguinal hernias
in children. Aust J Gen Pract. 2020;49(1–2):38–43.
6. Bowling K, Hart N, Cox P, Srinivas G. Management
of paediatric hernia. BMJ. 2017;359:1–6.
7. Öberg S, Andresen K, Rosenberg J. Etiology of
Inguinal Hernias: A Comprehensive Review. Front
Surg. 2017;4(September):1–8.
8. Weaver KL, Poola AS, Gould JL, Sharp SW,
St Peter SD, Holcomb GW 3rd. The risk of
developing a symptomatic inguinal hernia in
children with an asymptomatic patent processus
vaginalis. J Pediatr Surg 2017;52(1):60–64.
9. Swenson 0. Inguinal hernia. In: Raffensperger JC.
ed. Paediatric surgery 4th ed. New York: Appleton-
Century-Croft; 1980:107-20.
10. Chen Y-H, Wei C-H, Wang K-WK.
Children With Inguinal Hernia Repairs: Age
and Gender Characteristics. Glob Pediatr Heal.
2018;5(46):2333794X1881690.
11. Singh H, Wagh DD. Original article Management
of congenital inguinal hernia at A . V . B . R . H.
2016;5(4):13–23.
12. Pradhan GB, Shrestha D, Shrestha S, Bhattachan
CL. Inguinal herniotomy in children : a one year
survey at Nepal Medical. Nepal Med Coll J.
2011;13(4):301–2.
13. Rescorla FJ, Grosfeld JL. Inguinal hernia repair
in the perinatal period and early infancy: Clinical
considerations. J Pediatr Surg. 1984;19(6):832–7.
14. Ravikumar V, Rajshankar S, Hareesh
RSK,Nagendra GMR. A Clinical Study on the
Management of Inguinal Hernias in Children on the
General Surgical Practice. J Clin Diagn Res. 2013
Jan; 7(1): 144–147.