Abstract
Introduction:The overall rate of operative vaginal
delivery is diminishing, but the proportion of operative
vaginal deliveries conducted by vacuum is increasing. As
forceps assisted delivery requires more skill and has more
complications on maternal genital tract, this procedure is
being less frequently practiced. By the 1970s, the vacuum
extractor virtually replaced forceps for assisted deliveries
in most of the countries. Vacuum assisted vaginal delivery
reduces maternal as well as neonatal morbidity and
mortality in prolonged second stage of labor, non reassuring
fetal status and maternal conditions requiring a shortened
second stage.
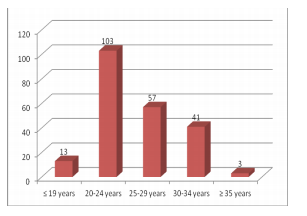
Materials and Methods: This was a record based
retrospective study of 217 vacuum assisted vaginal
deliveries conducted at Western Regional Hospital,
Pokhara for a period of one year. Patient’s discharge
charts were studied and details of indications for vacuum
application, maternal genital tract status, amount of
blood loss, postpartum hemorrhage (PPH), birth weight,
APGAR score at 1 and 5 minute, Neonatal Intensive Care
Unit (NICU) admission and neonatal death (NND) were
collected. Descriptive data analysis was done using SPSS
program.
Results:Out of the 8778 deliveries conducted during the
study period, 217 (2.47%) cases were vacuum assisted
vaginal deliveries. No significant adverse obstetrics
outcomes were noted. Most frequent indication was fetal
distress which accounted for 53.9%. Though 3rd/4th
degree perineal tears were less, episiotomy rate was higher
(69.1%). Regarding neonatal outcomes, mean APGAR
score at 5 minute was 7.42 ± 1.11 SD and 12.4% neonates
had APGAR score of less than 7 at 5 minute.
Conclusion:When standard criteria for vacuum application
are met and standard norms are followed, there is no
evidence of adverse obstetrics outcomes in vacuum assisted
vaginal delivery. Prompt delivery by a skilled clinician
in non reassuring fetal cardiac status reduces neonatal
morbidity and mortality.
References
Saidu AK, Ezeonu CT. Disappearing art of
forceps delivery and the trend of instrumental
vaginal deliveries at Abakaliki, Nijeria. Afr J
Med Health Sci. 2014; 13: 99-104.
2. WHO, UNICEF. Guidelines for monitoring the
availability and use of obstetric services. New
york: WHO, UNICEF, 1917.
3. Miksovsky P, Watson WJ. Obstetric vacuum
extraction: state of the art in the new
millennium. ObstetGynecolSurv 2001; 56:736.
4. Vacca A. Vacuum-assisted delivery: an analysis
of traction force and maternal and neonatal
outcomes. Aust N Z J ObstetGynaecol 2006;
46:124.
5. Johanson RB, Rice C, Doyle M, et al. A
randomised prospective study comparing the
new vacuum extractor policy with forceps
delivery. Br J ObstetGynaecol 1993; 100:524.
6. Baskett TF, Fanning CA, Young DC. A
prospective observational study of 1000
vacuum assisted deliveries with the OmniCup
device. J ObstetGynaecol Can 2008; 30:573.
7. Murphy DJ, Liebling RE, Patel R, et al. Cohort
study of operative delivery in the second stage
of labour and standard of obstetric care. BJOG
2003; 110:610.
8. American College of Obstetricians and
Gynecologists. Operative vaginal delivery.
ACOG Practice Bulletin number 17, American
College of Obstetricians and Gynecologists,
Washington, DC 2000.
9. Edozien LC. Towards safe practice in
instrumental vaginal delivery. Best Pract Res
ClinObstetGynaecol 2007; 21:639.
10. Kadas AS, Alliyu LD, Hauwa MA.
Instrumental delivery in Bauchi, Northest
Nigeria; J west Afr college surg. 2011: 1(4):
18-27
11. Noton F. International difference in the use of
obstetric interventions. JAMA. 1990; 263 (24):
3286-91.
12. Stern C, Permezel M, Petterson C, Lawson
J, Eggers T, Kloss M. The Royal Women’s
Hospital Family Birth Centre: the first 10 years
reviewed. Aust N Z J ObstetGynaecol. 1992;
32(4): 291-6.
13. Lukasse M, Qian P, Aamodt G. A midwife-led
birthing unit. Tidsskr Nor Laegeforen. 2006;
126(2): 170-2.
14. Penwell V. Mercy in action. Philippine birth
center statistics. Midwifery Today Int Midwife.
2004; 70: 56-57.
15. Lamichhane B, Singh A. Changing trends
of instrumental deliveries at Patan Hospital.
NJOG. 2015; 20 (2): 33-5.
16. de Leeuw JW, de Wit C, Kuijken JP, Bruinse
HW. Mediolateral episiotomy reduces the
risk for anal sphincter injury during operative
vaginal delivery. BJOG 2008; 115:104.
17. Murphy DJ, Macleod M, Bahl R, et al. A
randomised controlled trial of routine versus
restrictive use of episiotomy at operative
vaginal delivery: a multicentre pilot study.
BJOG 2008; 115:1695.
18. Robertson PA, Laros RK Jr, Zhao RL.
Neonatal and maternal outcome in low-pelvic
and midpelvic operative deliveries. Am J
ObstetGynecol 1990; 162:1436.